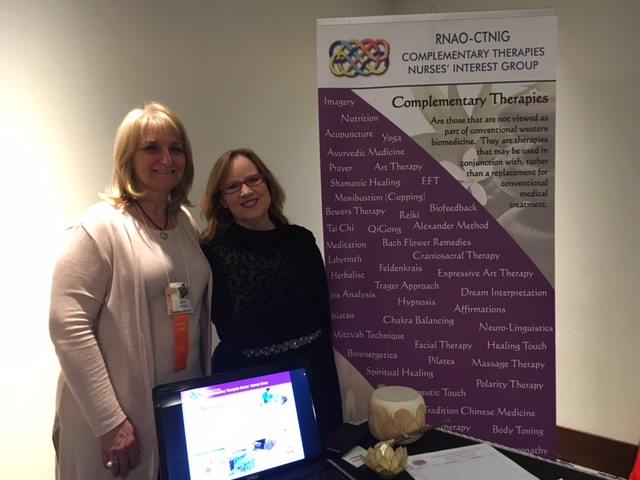
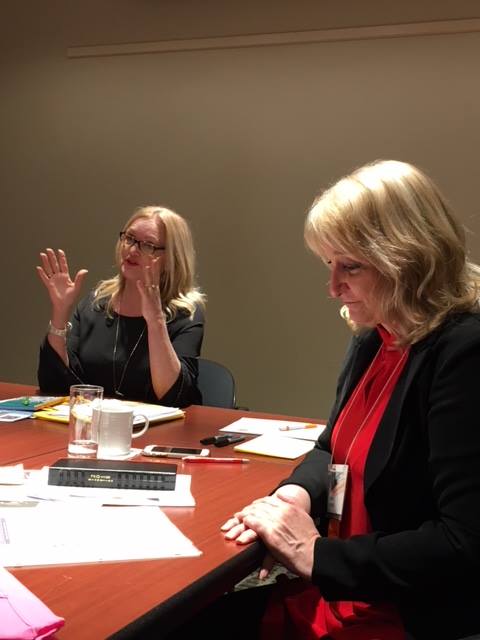
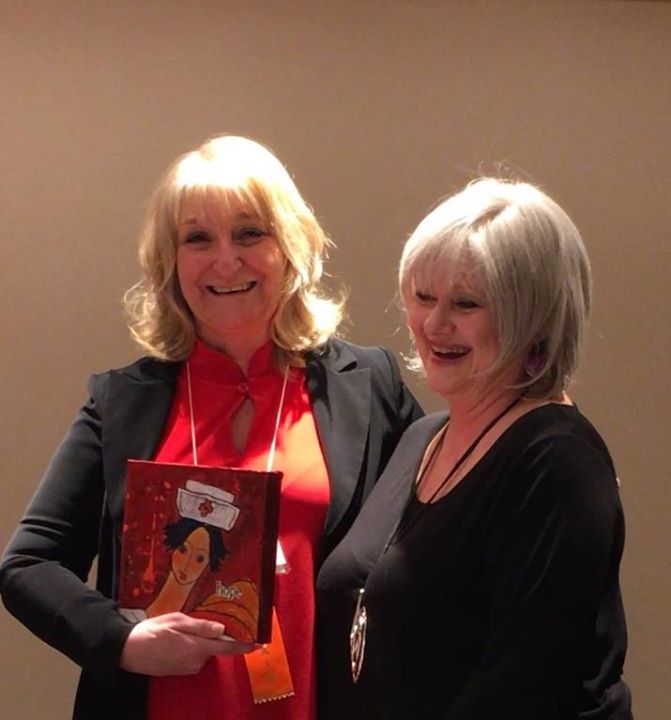
To our RNAO Community at the 100th AGM
- thank you for connecting with us! Please click on the image to download a copy of breathing practices. Please feel free to share this with your nursing team! For more way to benefit from holistic health approaches in your practice and personal life consider joining CTNIG